
What Is Skin Cancer? What Is Melanoma?
Melanoma is a malignant tumor of melanocytes. The tumors are generally found in the skin, but may also appear in the bowel and the eye (uveal melanoma). Melanoma is a type of skin cancer - one of the rarer types - but the cause of most skin cancer related deaths. Malignant melanoma is caused by an uncontrolled growth of skin pigment cells (melancytes). The word "melanoma" comes from the Ancient Greek melas meaning "black", and the Ancient Greek oma meaning "disease, morbidity".What is the difference between skin cancer and melanoma?
Melanoma is a type of skin cancer. Imagine the words bananas and fruit. All bananas (malignant melanoma)s are fruits (skin cancers), but not all fruits (skin cancers) are bananas (malignant melanomas). There are three main types of skin cancers: Basal Cell Carcinoma - Sometimes called non-melanoma skin cancer. It usually appears as a small, fleshy bump or nodule on the patient's hands, neck or head. Sometimes, the nodules may appear on the trunk of the body (mostly as flat growths). 90% of skin cancers are this type in the USA and UK. Basal cell carcinoma is easy to diagnose and is mostly easy to treat successfully. If left untreated it can spread to other parts of the body and can extend below the skin to the bone, causing significant local damage. People with basal cell carcinoma are at higher risk of developing other skin cancers.- Basal Cell Carcinoma is most commonly found among Caucasians. It very rarely occurs among dark-skinned patients. Among Caucasians, people with light hair, light colored eyes, and fair complexions are much more likely to get it, compared to Caucasions with darker colored eyes, hair and complexions.
- Squamous Ce ll Carcinoma -Sometimes referred to as non-melanoma carcinoma, it often appears as nodules on the skin. It is usually found on the rim of the ear, face, mouth and lips, but can also spread elsewhere in the body. It can also appear as red, scaly patches. It is generally found in the skin of Caucasian people, especially those with very fair skin. It is more aggressive than Basal Cell Carcinoma, but is still fairly easy to treat successfully.
- Malignant Melanoma - Cancer cells are found in the melanocytes - the pigment cells of the skin, also known as melanin. Although it is extremely rare in teenagers and children, there have been cases. It is predominately found in adults. This is the most aggressive form of skin cancer. Fortunately, it is also the rarest.
- Work. - CancerTherapyChina.com
75% of all skin cancer deaths are from malignant melanoma. It is most commonly found among fair-skinned people. However, people of all skin types can get it. Melanoma is not commonly found in parts of the body that are not covered by skin, such as the eyes, internal organs, vagina, large intestine, or mouth. A study found that a superfamily of molecules holds the secret to the development and spread of melanoma. - The rest of this article focuses on Malignant melanoma.
What are the symptoms of Malignant melanoma?
Malignant melanoma exists in a deeper layer of skin compared to other skins cancers. Experts say this is one of the reasons it is the most serious type of skin cancer. The deeper it starts from, the higher are the chances of it spreading.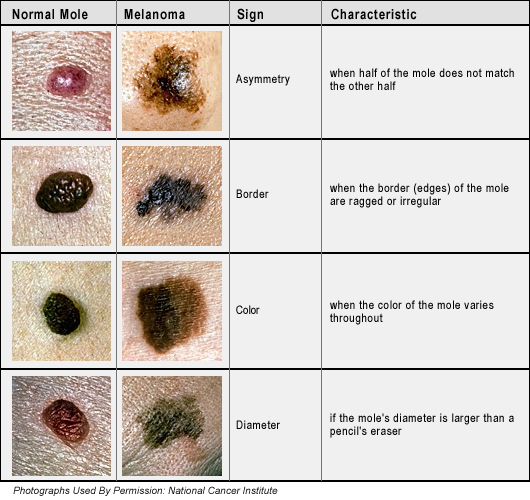
Patients mainly have melanomas on the back of the legs, arms and face. However, it can affect other locations too. The first signs of a melanoma could be: - A new mole appears.
- An existing mole changes in appearance from its usual single color and round/oval shape, not larger than ¼ of an inch (6mm) in diameter.
- Melanomas look like moles with an irregular shape. They tend to have more than just one color. They are generally larger than ¼ of an inch (6mm) in diameter.
- With some patients the melanoma may itch, and even bleed.
- Asymmetrical - the mole is not symmetrical, one half is different in shape from the other.
- Border - the border is ragged or notched. Most normal moles have regular borders.
- Colors - while most normal moles have just one color, melanomas often have two or more.
- Diameter - the diameter of a melanoma is greater than most moles (1/4 inch or 6mm)
- Elevation - when touched the melanoma will feel slightly raised above the skin
A study revealed that dermatologists depend on overall pattern recognition and comparison rather than specific analytic criteria to distinguish melanoma lesions (malignant skin cancer) from harmless skin moles.
What causes malignant melanoma?
When the structure of DNA in human cells change cancer can begin - we call this genetic mutation. Each of our cells is programmed to carry out many functions; this programming (set of instructions) is in the DNA. The instructions can be to grow, reproduce, auto-destruct, etc.When the DNA alters and instructions change, sometimes cells start to reproduce at an uncontrollable speed - lumps start to appear; these lumps are tumors. If the tumor is left untreated it can grow rapidly and spread to other parts of the body. When cancer does spread, it usually does so through the lymphatic system. The lymphatic system includes sever al glands around the body. As soon as the cancer reaches the lymphatic system it has access to several other parts of the body.
Experts say that over-exposure to sunlight is the main cause of malignant melanomas. Sunlight has large amounts of radiation in the form of light and heat. The atmosphere of this planet filters out most of the harmful effect of this radiation. Two radiation wavelengths, however, still get through and hit our skin - UVA (ultraviolet A) and UVB (ultraviolet B). UVA is the one that causes mutations in our melanocytes. Melanocytes produce melanin; a substance that gives color to our skin. If the mutated melanocytes become mutated (their DNA alters) melanomas can develop. UVB can also cause other non-melanoma types of skin cancer.
Artificial sunlamps - those found in tanning beds - also produce UVA. If they are used excessively they can increase a person's risk of developing melanomas.
Who is at high risk of developing malignant melanoma?
The following people have a higher risk of developing malignant melanoma:- Those with a history of blistering sunburns as a teenager.
- Those who had outdoor summer jobs for three or more years as a teenager.
- People with pale skin, especially skin that does not tan easily (goes red instead).
- People with red hair.
- People with blond hair.
- People with light eyes (blue).
- People with many moles.
- People with many freckles.
- A genetic variation leads to a nearly four-fold increase of melanoma in women under the age of 50, researchers have revealed.
- People with HIV or any condition that lowers their immune system.

- People taking immunosuppressants (medicines to lower your immune system).
- People who have a family history of melanoma. Researchers found that people with a family history of the skin cancer melanoma show reductions in anxiety and depression after getting tested for a high-risk gene mutation.
A study revealed that mobile phone (cell phone) use is not associated with the risk of melanoma of the eye.
How i
s malignant melanoma diagnosed?
Anybody who detects a mole that looks different from before should see their GP (general practitioner, primary care physician) immediately. The doctor will look at the patient's skin and determine whether further assessment is required. In the UK it is common for a GP to take a digital photograph of an unusual-looking mole and to email it to a skin specialist (dermatologist).If the doctor suspects there may be something unusual he will usually refer the patient to a dermatologist. The dermatologist will most likely perform a biopsy - the mole is removed and examined under a microscope to find out whether it has cancerous cells in it.
If the biopsy indicates there are cancerous cells, the doctor may carry out further biopsies on the lymph nodes nearest to where the mole was.
If the doctor wants to find out whether the cancer might have spread into other parts of the body, he/she may carry out:
- Blood tests
- A chest X-ray
- An MRI (magnetic resonance imaging) scan
- A CT (computerized tomography) scan
What are the stages of malignant melanoma?
Most dermatologists refer to 4 stages of melanoma:- Stage 1 - The melanoma is just on the surface of the skin. It is less than 2mm thick (less than 1/10th of an inch).
- Stage 2 - The melanoma is still just on the surface of the skin. However, it is over 2mm thick. There may be other small pockets of cancerous cells near the main melanoma.
- Stage 3 - The melanoma has reached nearby lymph nodes. Cancerous cells are present which are further away than 5cm (2 inches) from the main melanoma.
- Stage 4 - Melanoma cells have spread elsewhere in the body, such as the brain or the lungs.
What is the treatment for malignant melanoma?
Dermatologists say that when melanoma is diagnosed in its earliest, most treatable stages, time is on your side. A study explained why early diagnosis and regular skin exams are vital for beating melanoma.Compounds that exist in green vegetables, such as broccoli or cabbage could be a powerful drug against melanoma, say researchers from Penn State College of Medicine.
Treatment for malignant melanoma depends on several factors, the patient's..:
- Age
- General health
- Stage of cancer
- Personal preferences
Treating early-stage melanoma treatment - Stage 1 Melanoma
- Surgical removal
In many cases, all that is needed is the removal of the melanoma (surgical excision), and that's it. If the melanoma is very thin it is most likely that all of it was removed during the biopsy and no further treatment is required. Most surgeons will take out the cancer as well as a small border of normal skin and a layer of tissue below the skin to optimize the chances that all the cancer is eliminated.
Surgeons used to more commonly take out a large border of skin and then the patient would have skin graft. However, it seems that if the surgeon takes out smaller amounts of healthy tissue this is just as effective for many cases of invasive melanomas. The advantage of not taking out too much healthy tissue is that a skin graft is not required.
- Surgical removal and possible rem oval of nearby lymph nodes
As well as removing any affected area of skin, sometimes the surgeon has to remove a nearby lymph nodes as well in case cancerous cells are present there - this is called a block dissection and the patient is given a general anesthetic. If lymph nodes are removed there is a risk that the patient's lymphatic system will be disrupted and he/she can develop lymphedema. Lymphedema patients experience a build-up of fluids in their limbs. - Interferon
After surgery the patient may be given interferon. Interferon can reduce the chances of melanoma recurrence. Interferon encourages the body's immune system to fight off any remaining cancer cells. Most patients are given three interferon injections each week. M any patients can learn how to inject themselves - meaning they do not have to leave home for treatment. How long this treatment lasts depends on several factors, including how advanced the melanoma is.
Interferon treatment may have the following side effects, which can be quite bad at first:- Chills
- Fever
- Joint pain
- Tiredness (fatigue) The following side effects are also possible, but less common:
- Vomiting
- Nausea
- Irritation at injection site
- Hair loss
- Pins and needles in the hands and toes
- Depression
- Mood changes
- Infertility
- Higher susceptibility to infection
- Alterations in heart rhythm
- Alterations in blood pressure
After the second and third doses the side effects start to subside. Patients should report any less common side-effects to their doctor, who may consider offering another treatment. Most patients are monitored closely while on interferon treatment, this may include regular blood tests, urine tests, and blood pressure checks.
At this point the chances of a cure are improbable. However, it is possible to slow down progression of the cancer and help the patient to live longer. The following treatments are available:
- Interferon treatment (details above in Stage 2 and 3 treatments).
- Chemotherapy - cells are destroyed with the aid of drugs. Doctors will usually administer at least two drugs simultaneously, either intravenously, orally or both. Chemotherapy, which is often resistant to melanoma, is sometimes used to relieve the symptoms of patients with advanced metastatic melanoma.
Side effects may include:- Nausea
- Vomiting
- Hair loss
- Tiredness (fatigue)
- Weakened immune system
In the vast majority of cases symptoms will subside as soon as treatment has finished. - Radiation therapy (radiotherapy) - High energy X-rays are targeted at the cancer cells and destroy them. Radiotherapy is also used to relieve symptoms of patients with advanced metastatic melanoma.
Side effects may include:- Tiredness (fatigue)
- Loss of appetite
- Hair loss
- Sore skin
- Lower libido (lack of interest in sex)
- Nausea
Side effects may persist for several weeks, or even months after treatment has stopped.
- Clinical trials - some doctors may suggest participating in a clinical trial. A clinical trial is a study of a drug that has not yet been approved by the regulatory authorities. It usually involves a certain number of participants who either take the trial drug, an existing drug, or a placebo. Anyone who enrolls in a clinical trial has the opportunity to try out evolving therapies. The downside is that the outcome is unclear, as well as the side effects. Currently (June 2009) the following therapies are in clinical trials for malignant melanoma: chemoimmunotherapy, gene therapy, targeted therapy, and vaccine treatment.
What are the complications of malignant melanoma?
- Recurrence
People who have had malignant melanomas are at a higher risk of future occurrences of malignant melanomas. The further advanced the previous melanoma was the higher the chances of recurrences are. If a doctor determines that a patient is at high risk of recurrence he/she will be checked regularly. The patient will also be taught how to self-check for signs and symptoms. - Parkinson's Disease
People with a family history of melanoma may have a greater risk of developing Parkinson's disease, a study found.
Prevention
- Avoid the sun at peak times - this means staying out of the sun's rays between 10am and 4pm. Perhaps outdoor activities could take place at other times of the day. Clouds do not protect you.
- Sunscreen - sunscreens are effective at blocking harmful rays. However, they do not block them all out. Dermatologists say sunscreens should form a part of your prevention strategy.
- Wear a hat - remember that a baseball type cap does not protect the tips of the ear. Broad-brimmed hats provide better protection.
- Wear sunglasses - they must be sunglasses than block both UVA and UVB rays.
- Avoid tanning beds - UVA rays penetrate deeper into the skin and cause precancerous skin lesions.
- Be aware with some medications - some medications may make the skin more sensitive to sunlight. These may include medications for diabetes, hypertension (high blood pressure), cholesterol control, contraceptives, ibuprofen, and some acne medications. If you are taking a medication that makes your skin more sensitive to sunlight be extra careful.

- Regularly check your skin - everybody should examine their skin for any unusual growths, colors or shapes, especially in existing moles, freckles or birthmarks. Regular visits to the doctor for a check up after the age of 40 are recommended.
I was diagnosed of Herpes 2years ago and I have tried all possible means to get the cure but all to no avail, until i saw a post in a health forum about a Herbal Doctor(Dr imoloa who prepares herbal medicine to cure all kind of diseases including Herpes, at first i doubted, if it was real but decided to give him a trial, when i contacted Dr imoloa through his Email: drimolaherbalmademedicine@gmail.com he guided me and prepared a herbal medicine and sent it to me via courier Delivery service,when i received the package (herbal medicine) He gave me instructions on how to consume it, i started using it as instructed and i stop getting outbreaks and the sores started vanishing, could you believe i was cured of this deadly virus within two to three weeks and notices changes in my body. Days of using this REMEDY,couldn't believe the healing at first until i see it as my HERPES get cleared like magic Dr imoloa also use his herbal medicine to cure diseases like, HIV/aids, lupus disease, dry cough, fever, malaria, bronchitis disease, cystic fibrosis, Lyme disease, acute myeloid leukaemia, alzheimer's disease, blood poisoning, measles, kidney cancer, kidney infections, diarrhoea, epilepsy, joint pain, mouth ulcer,bowel cancer, discoid eczema, eye cancer, food poisoning, fibroid, hairy cell leukaemia, mouth cancer, skin disease, lung cancer, rheumatoid lung disease, liver disease, penile cancer, parkinson disease, arthritis, breast cancer, bone cancer hepatitis A.B.C, Diabetes, fatigue, muscle aches, anal cancer, asthma, Contact this great herbal Doctor today the father of herbalism. via Email: drimolaherbalmademedicine@gmail.com or whatssapp him +2347081986098. and get cured permanently He is real..
ReplyDeleteAll thanks to Doctor James herbal mix medicine for using his herbal medicine to cure my MELANOMA DISEASE I suffered for years and it almost circulated all over my body and I seek for natural treatment. I found on the internet that Dr James uses his herbal medicine to cure many of people from the virus and I contacted him on his Email [drjamesherbalmix@gmail.com]. And he said he is going to help me ,after 2 days of reaching him.he prepared his herbal soap and medicine ans sent to me,and I used the medicine as he told me for 15 days,my skin cancer was cued and disappeared just as he told me it will after the use of his medicine which i never doubted him . At least his treatment cured me completely from melanoma disease. Hopefully it will be helpful for you as it happened with me. Dr. James herbal medicine is made of natural herbs, with no side effects, and easy to drink. I'm shearing my testimony to reach out to anyone suffering from this horrible skin virus should contact. or any type of human illness, including HIV / AIDS, herpes,cancer,Ovarian Cancer,Pancreatic cancers, bladder cancer,skin cancer, prostate cancer, Glaucoma., Cataracts,Macular degeneration,Cardiovascular disease,Autism,Lung disease. Enlarged prostate,Osteoporosis. Alzheimer's disease,psoriasis ,Tach Diseases,Lupus,
ReplyDeleteDementia.kidney cancer, lung cancer, skin cancer, skin cancer and skin cancer.testicular Cancer, , LEUKEMIA, HEPATITIS, INFERTILITY WOMEN /.CONTACT EMAIL : drjamesherbalmix@gmail.com