What Is Alzheimer's Disease? What Causes Alzheimer's Disease?
Alzheimer's disease is a progressive neurologic disease of the brain leading to the irreversible loss of neurons and the loss of intellectual abilities, including memory and reasoning, which become severe enough to impede social or occupational functioning. Alzheimer's disease is also known as simply Alzheimer's, and Senile Dementia of the Alzheimer Type (SDAT) .
During the course of the disease plaques and tangles develop within the structure of the brain. This causes brain cells to die. Patients with Alzheimer's also have a deficiency in the levels of some vital brain chemicals which are involved with the transmission of messages in the brain - neurotransmitters.

Alzheimer's disease is the most common form of dementia. The disease gets worse as it develops - it is a progressive disease. There is no current cure for Alzheimer's, although there are ways of slowing down its advance and helping patients with some of the symptoms. Alzheimer's is also a terminal disease - it is incurable and causes death.
According the National Institute on Aging, there are estimated to be between 2.4 million and 4.5 million Americans who have Alzheimer's. There are approximately 417,000 people in the UK with Alzheimer's, according to the Alzheimer's Society.
Why the name Alzheimer's disease? Aloysius Alzheimer and Emil Kraepelin, Germany
Aloysius Alzheimer was a German neuropathologist and psychiatrist. He is credited with identifying the first published case of "presenile dementia" in 1906, which Kraepelin later identified as Alzheimer's disease - naming it after his colleague.In 1901, while he worked at the city mental asylum in Frankfurt am Main, Germany, Dr. Alzheimer had a 51 year old patient called Mrs. Auguste Deter. The patient had distinct behavioral symptoms which did not fit any existing diagnoses - she had rapidly failing memory, disorientation, confusion, had trouble expressing her thoughts, and was suspicious about her family members and the hospital staff. Her symptoms progressed relentlessly. Dr. Alzheimer wrote that she once said to him "I have lost myself."
Over the coming years Auguste Deter would take up more and more of Dr. Alzheimer's time, to the point of almost becoming an obsession for him. The lady died in 1906 and Dr. Alzheimer, who was working at Kraepelin's lab in Munich, had her patient records and brain sent there.
Along with two Italian doctors, Dr. Alzheimer performed an autopsy. The autopsy revealed that her brain had shrunken dramatically, but there was no evidence of atherosclerosis (thickening and hardening of the walls of the arteries). He used a silver staining technique he had learnt from ex-colleague Franz Nissl which identified amyloid plaques and neurofribrillary tangles in the brain - two hallmarks of the disease.
In November, 1906 Dr. Alzheimer gave the first lecture ever that presented the pathology and the clinical symptoms of presenile dementia together. Kraepelin started using the term Alzheimer's disease, which by 1911 was being used throughout Europe and by European doctors when diagnosing patients in the USA.
Fairly recently, Dr. Alzheimer's findings were reevaluated when his original microscope preparations on which he based his description of the disease were rediscovered in Munich.
A researcher from Prague, Oskar Fischer, and a contemporary of Dr. Alzheimer's, may have described the pathology of dementia in greater depth than did Alzheimer himself, say Czech scientists who have been digging through historical archives in Prague.
What are the symptoms of Alzheimer's disease?
Doctors say Alzheimer's disease can sometimes be tricky to diagnose because each patient has unique signs and symptoms. Several of the signs and symptoms present in Alzheimer's disease also exist in other conditions and diseases.Alzheimer's disease is classified into several stages. Some doctors use a 7-stage framework, while others may use a 4, 5 or 6-stage one.
A common framework includes 1. Pre-Dementia Stage. 2. Mild Alzheimer's Stage. 3. Moderate Alzheimer's Stage. 4. Severe Alzheimer's Stage. The example below is of a 7-stage framework.
The 7 stages of diagnostic framework
Most patients take from 8 to 10 years to progress through all the seven stages. However, some may live for 20 years after neuron changes first occur.
Stage 1 - No impairment
Memory and cognitive abilities seem to be normal. During a medical interview a health care professional identifies no evidence of memory or cognitive problems.
Stage 2 - Minimal Impairment (Very Mild Cognitive Decline)
Could be normal age-related changes, or the earliest signs of Alzheimer's.
Friends, family and health care professionals hardly notice any memory lapses. Approximately 50% of people aged 65 and over start experiencing slight difficulties with recalling the occasional word and concentration. The person may feel there are occasional memory lapses, such as forgetting familiar words or the names, and perhaps where they left their keys, glasses or some other everyday object.
Stage 3 - Early Confusional (Mild Cognitive Decline). Duration - 2 to 7 years.
Early-stage Alzheimer's is sometimes diagnosed at this stage.
- The patient has slight difficulties which have some impact on certain everyday functions. In many cases the patient will try to conceal the problems.
- Problems include difficulties with word recall, organization, planning, mislaying things, failing to remember recently learned data which may cause problems at work and at home - family members and close associates become aware.
- Problem reading a passage and retaining information from it.
- The ability to learn new things may be affected.
- Problems with organization.
- Moodiness, anxiety, and in some cases depression.
With these symptoms diagnosis is easy to confirm.
- Still identifies familiar people and is aware of self.
- Reduced memory of personal history.
- Problems with numbers which impact on family finance - managing bills, checkbooks, etc. Previously doable numerical exercises, such as counting backwards from 88 in lots of 6s become too difficult.
- Knowledge of recent occasions or current events is decreased.
- Sequential tasks become more difficult, including driving, cooking, planning dinner for guests, many domestic chores, shopping alone, and reading and then selecting what is in a menu at the restaurant.
- Withdraws from conversations, social situations, and mentally challenging situations.
- Denies there is a problem and becomes defensive.
- Requires help with some of the more complicated aspects of independent living.
- Cognitive deterioration is more serious.
- Cannot survive independently in the community and requires some assistance with day-to-day activities.
- Cannot remember details about personal history, such as name of where they went to school, telephone numbers, personal address, etc.
- Confused about what day it is, month, year.
- Confused about where they are or where things are.
- Problems with numbers; mathematical abilities get worse.
- Easy prey for scammers.
- Require supervision and sometimes help when dressing, including selecting right clothing for the season or occasion.
- Require help carrying out some daily living tasks.
- Can still eat and go to the toilet unaided.
- Unable to recall current information consistently.
- Usually remember substantial amounts about themselves, such as their name, name of spouse and children.
Memory continues to deteriorate. There is a considerable change in personality. Require all-round help with daily activities.
- Virtually totally unaware of present and most recent experiences.
- Cannot recall personal history very well.
- Can still usually recall their own name.
- Know family members are familiar but cannot recall their names.
- Can communicate pleasure and pain nonverbally.
- Ability to dress progressively deteriorates. Need help dressing and undressing.
- Ability to bathe and wash self progressively deteriorates.
- Fecal and/or urinary incontinence more likely.
- Need help when going to the toilet - flushing, wiping, disposing of tissues.
- Disruption of sleep patterns.
- Wander off and become lost.
- Suspicious, paranoid, aggressive. May believe caregiver is an impostor, devious, scheming, cunning, dishonest.
- Repeat words, phrases or repetitively utters sounds.
- Repetitive/compulsive behavior, such as tearing up tissues or wringing hands.
- Disturbed, agitated, especially later on in the day.
- Hallucinations, also more common later on in the day. May hear, smell or see things that are not there.
- Eventually need care and supervision, but can respond to non-verbal stimuli.
During the last stage of Alzheimer's disease patients lose the ability to respond to their environment, they cannot speak, and eventually cannot control movement. The duration of this stage may depend on the quality of care the patient receives.
- Severely limited cognitive ability.
- Patients lose their ability to recognize speech, but may utter short words or moans to communicate.
- Usually the ability to walk unaided is lost first, then the ability to sit unaided, plus the ability to smile, and eventually the ability to hold the head up.
- Body systems start to fail and health deteriorates.
- Swallowing becomes increasingly more difficult. Chocking when eating/drinking becomes more common.
- Reflexes become abnormal.
- Seizures are possible.
- Muscles grow rigid.
- Generally bedridden.
- Spends more time asleep.
- Require round-the-clock care.


 uses Muscular Dystrophy?
uses Muscular Dystrophy?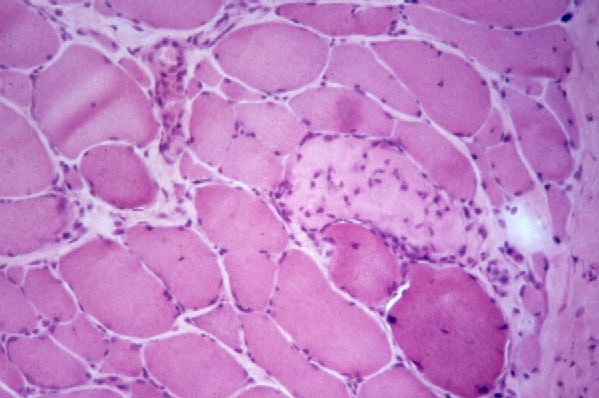







 asmodium falciparum (80% of cases), Plasmodium vivax, Plasmodium ovale, Plasmodium malariae. Affects the red blood cells. Exists in tropical regions. Transmitted by the anopheles mosquito.
asmodium falciparum (80% of cases), Plasmodium vivax, Plasmodium ovale, Plasmodium malariae. Affects the red blood cells. Exists in tropical regions. Transmitted by the anopheles mosquito.