Rheumatic Fever
Rheumatic fever is an inflammatory disease that may develop after an infection with Streptococcus bacteria (such as strep throat or scarlet fever). The disease can affect the heart, joints, skin, and brain.Acute rheumatic fever commonly appears in children between the ages of 5 and 17, with only 20% of first-time attacks occurring in adults. The illness is so named because of its similarity in presentation to rheumatism.
Causes,Risk Factors:
Rheumatic fever is common worldwide and is responsible for many cases of damaged heart valves. It is not common in the United States, and usually occurs in isolated outbreaks.Rheumatic fever mainly affects children ages 6 -15, and occurs approximately 20 days after strep throat or scarlet fever.
Symptoms:
- Abdominal pain
- Fever
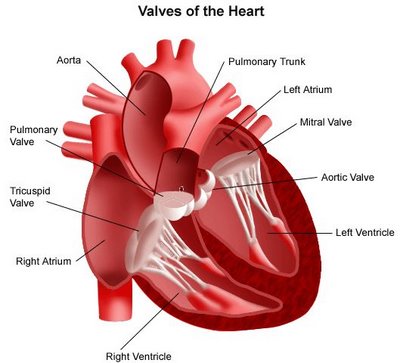
- Heart (cardiac) problems, which may not have symptoms, or may result in shortness of breath and chest pain
- Joint pain, arthritis (mainly in the knees, elbows, ankles, and wrists)
- Joint swelling; redness or warmth
- Nosebleeds (epistaxis)
- Skin nodules
- Skin rash (erythema marginatum)
- Skin eruption on the trunk and upper part of the arms or legs
- Eruptions that look ring-shaped or snake-like.
Tests may include:
- Blood test for recurrent strep infection (such as an ASO test)
- Complete blood count
- Electrocardiogram
- Sedimentation rate (ESR)
Infection:
Patients with positive cultures for Streptococcus pyogenes should be treated with penicillin as long as allergy is not present. This treatment will not alter the course of the acute disease.
The most appropriate treatment stated in the Oxford Handbook of Clinical Medicine for rheumatic fever is benzylpenicillin.
Heart Failure:
Some patients develop significant carditis which manifests as congestive heart failure. This requires the usual treatment for heart failure: diuretics and digoxin. Unlike normal heart failure, rheumatic heart failure responds well to corticosteroids.
Pathophysiology:
Rheumatic fever is a systemic disease affecting the peri-arteriolar connective tissue and can occur after an untreated Group A Beta hemolytic streptococcal pharyngeal infection. It is believed to be caused by antibody cross-reactivity. This cross-reactivity is a Type II hypersensitivity reaction and is termed molecular mimicry. Usually, self reactive B cells remain anergic in the periphery without T cell co-stimulation. During a Streptococcus infection, mature antigen presenting cells such as B cells present the bacterial antigen to CD4-T cells which differentiate into helper T2 cells. Helper T2 cells subsequently activate the B cells to become plasma cells and induce the production of antibodies against the cell wall of Streptococcus. However the antibodies may also react against the myocardium and joints, producing the symptoms of rheumatic fever
Treatment:
If you are diagnosed with acute rheumatic fever you will be treated with antibiotics.
Anti-inflammatory medications such as aspirin or corticosteroids reduce inflammation to help manage acute rheumatic fever.
You may have to take low doses of antibiotics (such as penicillin, sulfadiazine, or erythromycin) over the long term to prevent strep throat from returning.
Prevention:
The most important way to prevent rheumatic fever is by getting quick treatment for strep throat and scarlet fever.
Anti-inflammatory medications such as aspirin or corticosteroids reduce inflammation to help manage acute rheumatic fever.
You may have to take low doses of antibiotics (such as penicillin, sulfadiazine, or erythromycin) over the long term to prevent strep throat from returning.
Prevention:
The most important way to prevent rheumatic fever is by getting quick treatment for strep throat and scarlet fever.