
Back pain is a very common complaint. According to the Mayo Clinic, USA, approximately 80% of all Americans will have low back pain at least once in their lives. Back pain is a common reason for absence from work, or visiting the doctor's.
According to the NHS (National Health Service), UK, back pain is the largest cause of work-related absence in the United Kingdom. Although back pain may be painful and uncomfortable, it is not usually serious.
Even though back pain can affect people of any age, it is significantly more common among adults aged between 35 and 55 years.
Experts say that back pain is associated with the way our bones, muscles and ligaments in our backs work together.
Pain in the lower back may be linked to the bony lumbar spine, discs between the vertebrae, ligaments around the spine and discs, spinal cord and nerves, lower back muscles, abdomen and pelvic internal organs, and the skin around the lumbar area. Pain in the upper back may be due to disorders of the aorta, tumors in the chest, and spine inflammation.
 What are the risk factors for back pain?
What are the risk factors for back pain?
A risk factor is something which increases the likelihood of developing a condition or disease. For example, obesity significantly raises the risk of developing diabetes type 2. Therefore, obesity is a risk factor for diabetes type 2. The following factors are linked to a higher risk of developing low back pain: - A mentally stressful job
- Pregnancy - pregnant women are much more likely to get back pain
- A sedentary lifestyle
- Age - older adults are more susceptible than young adults or children
- Anxiety
- Depression
- Gender - back pain is more common among females than males
- Obesity/overweight
- Smoking
- Strenuous physical exercise (especially if not done properly)
- Strenuous physical work
What are the signs and symptoms of back pain?
A symptom is something the patient feels and reports, while a sign is something other people, such as the doctor detect. For example, pain may be a symptom while a rash may be a sign.The main symptom of back pain is, as the name suggests, an ache or pain anywhere on the back, and sometimes all the way down to the buttocks and legs. In most cases signs and symptoms clear up on their own within a short period.
If any of the following signs or symptoms accompanies a back pain your should see your doctor:
- Weight loss
- Elevated body temperature (fever)
- Inflammation (swelling) on the back
- Persistent back pain - lying down or resting does not help
- Pain down the legs
- Pain reaches below the knees
- A recent injury, blow or trauma to your back
- Urinary incontinence - you pee unintentionally (even small amounts)
- Difficulty urinating - passing urine is hard
- Fecal incontinence - you lose your bowel control (you poo unintentionally)
- Numbness around the genitals
- Numbness around the anus
- Numbness around the buttocks
- People aged less than 20 and more than 55 years
- Patients who have been taking steroids for a few months
- Drug abusers
- Patients with cancer
- Patients who have had cancer
- Patients with low immune systems
What are the causes of back pain?
The human back is composed of a complex structure of muscles, ligaments, tendons, disks and bones - the segments of our spine are cushioned with cartilage-like pads. Problems with any of these components can lead to back pain. In some cases of back pain, its cause is never found. Back Pain Treatment - San Joaquin's Orthopedic Leader. 5+ Years of Excellence. Call Today! - www.SPOC-Ortho.com
Egoscue - Pain Free Back - Relieve back pain through simple exercises. Avoid drugs and surgery. - www.egoscue.com
Arthritis Hospital China - Ms. Rahma could walk again after stay on the w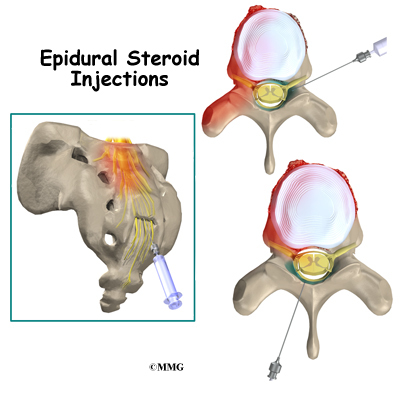 heelchair for 7 years. - www.tcmtreatment.com
heelchair for 7 years. - www.tcmtreatment.com
Miyon Hospital Pakistan - Mr.Aadil could walk again stay on the wheelchair for 5 years.-
www.medicalphase.blogspot.com
Egoscue - Pain Free Back - Relieve back pain through simple exercises. Avoid drugs and surgery. - www.egoscue.com
Arthritis Hospital China - Ms. Rahma could walk again after stay on the w
 heelchair for 7 years. - www.tcmtreatment.com
heelchair for 7 years. - www.tcmtreatment.comMiyon Hospital Pakistan - Mr.Aadil could walk again stay on the wheelchair for 5 years.-
www.medicalphase.blogspot.com
- Strained muscles
- Strained ligaments
- Lifting something improperly
- Lifting something that is too heavy
- The result of an abrupt and awkward movement
- A muscle spasm
- Ruptured disks - each vertebra in our spine is cushioned by disks. If the disk ruptures there will be more pressure on a nerve, resulting in back pain.
- Bulging disks - in much the same way as ruptured disks, a bulging disk can result in more pressure on a nerve.
- Sciatica - a sharp and shooting pain that travels through the buttock and down the back of the leg, caused by a bulging or herniated disk pressing on a nerve.
- Arthritis - patients with osteoarthritis commonly experience problems with the joints in the hips, lower back, knees and hands. In some cases spinal stenosis can develop - the space around the spinal cord narrows.
- Abnormal curvature of the spine - if the spine curves in an unusual way the patient is more likely to experience back pain. An example is scoliosis, when the spine curves to the side.
- Osteoporosis - bones, including the vertebrae of the spine, become brittle and porous, making compression fractures more likely.
- Cauda equina syndrome - the cauda equine is a bundle of spinal nerve roots that arise from the lower end of the spinal cord. People with cauda equine syndrome feel a dull pain in the lower back and upper buttocks, as well as analgesia (lack of feeling) in the buttocks, genitalia and thigh. There are sometimes bowel and bladder function disturbances.
- Cancer of the spine - a tumor located on the spine may press against a nerve, resulting in back pain.
- Infection of the spine - if the patient has an elevated body temperature (fever) as well as a tender warm area on the back, it could be caused by an infection of the spine.
- Other infections - pelvic inflammatory disease (females), bladder or kidney infections.
- Sleep disorders - individuals with sleep disorders are more likely to experience back pain, compared to others.
- Shingles - an infection that can affect the nerves.
- Bad mattress - if a mattress does not support specific parts of the body and keep the spine straight, there is a greater risk of developing back pain.
Back pain can also be the result of some everyday activity or poor posture. Examples include:
- Bending awkwardly
- Pushing something
- Pulling something
- Carrying something
- Lifting something
- Standing for long periods
- Bending down for long periods
- Twisting
- Coughing
- Sneezing
- Muscle tension
- Over-stretching
- Sitting in a hunched position for long periods (e.g. when driving)
- Long driving sessions without a break (even when not hunched)
Diagnosing back pain
Most GPs (general practitioners, primary care physicians) will be able to diagnose back pain after carrying out a physical examination, and interviewing the patient. In the majority of cases imaging scans are not required.If the doctor and/or patient suspect some injury to the back, tests may be ordered. Also, if the doctor suspects the back pain might be due to an underlying cause, or if the pain persists for too long, further tests may be recommended.
Suspected disc, nerve, tendon, and other problems - X-rays or some other imaging scan, such as a CT (computerized tomography) or MRI (magnetic resonance imaging) scan may be used to get a better view of the state of the soft tissues in the patient's back.
- X-rays can show the alignment of the bones and whether the patient has arthritis or broken bones. They are not ideal for detecting problems with muscles, the spinal cord, nerves or disks.
- MRI or CT scans - these are good for revealing herniated disks or problems with tissue, tendons, nerves, ligaments, blood vessels, muscles and bones.
- Bone scan - a bone scan may be used for detecting bone tumors or compression fractures caused by brittle bones (osteoporosis). The patient receives an injection of a tracer (a radioactive substance) into a vein. The tracer collects in the bones and helps the doctor detect bone problems with the aid of a special camera.
- Electromyography or EMG - the electrical impulses produced by nerves in response to muscles is measured. This study can confirm nerve compression which may occur with a herniated disk or spinal stenosis (narrowing of the spinal canal).
Chiropractic, Osteopathy and Physical Therapy (UK: Physiotherapy)
- A chiropractor - the chiropractor will diagnose by touching (palpitation) and a visual inspection. Chiropractic is known as a direct approach, with a strong focus on the adjustments of the spinal joints. Most good chiropractors will also want to see imaging scan results, as well as blood and urine tests.
- An osteopath - the osteopathic approach also diagnoses by touching and a visual inspection. Osteopathy involves slow and rhythmic stretching (mobilization), pressure or indirect techniques and manipulations on joints and muscles.
- A physical therapist (UK: physiotherapist) - a physical therapist's training focuses on diagnosing problems in the joints and soft tissues of the body.
What are the treatment options for back pain?
In the vast majority of cases back pain resolves itself without medical help - just with careful attention and home treatment. Pain can usually be addressed with OTC (over-the-counter, no prescription required) painkillers. Resting is helpful, but should not usually last more than a couple of days - too much rest may actually be counterproductive.Usually back pain is categorized into two types:
- Acute - back pain comes on suddenly and persists for a maximum of three months.
- Chronic - the pain gradually develops over a longer period, lasts for over three months, and causes long-term problems.
If home treatments do not give the desired results, a doctor may recommend the following:
Medication - back pain that does not respond well to OTC painkillers may require a prescription NSAID (nonsteroidal anti-inflammatory drug). Codeine or hydrocodone - narcotics - may also be prescribed for short periods; they require close monitoring by the doctor.
Some tricyclic antidepressants, such as amitriptyline, have been shown to alleviate the symptoms of back pain, regardless of whether or not the patient has depression.
Physical Therapy (UK: physiotherapy) - the application of heat, ice, ultrasound and electrical stimulation, as well as some muscle-release techniques to the back muscles and soft tissues may help alleviate pain. As the pain subsides the physical therapist may introduce some flexibility and strength exercises for the back and abdominal muscles. Techniques on improving posture may also help. The patient will be encouraged to practice the techniques regularly, even after the pain has gone, to prevent back pain recurrence.
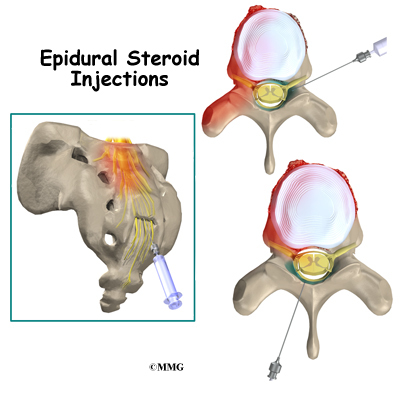
Cortisone injections - if the above-mentioned therapies are not effective enough, or if the pain reaches down to the patient's legs, cortisone may be injected into the epidural space (space around the spinal cord). Cortisone is an anti-inflammatory drug; it helps reduce inflammation around the nerve roots. According to The Mayo Clinic, USA, the pain-relief effect will wear off after less than six weeks.
Injections may also be used to numb areas thought to be causing the pain. Botox (botulism toxin), according to some early studies, are thought to reduce pain by paralyzing sprained muscles in spasm. These injections are effective for about three to four months.
Surgery - surgery for back pain is very rare. If a patient has a herniated disk surgery may be an option, especially if there is persistent pain and nerve compression which can lead to muscle weakness. Examples of surgical procedures include:
- Fusion - two vertebrae are joined together, with a gone graft inserted between them. The vertebrae are splinted together with metal plates, screws or cages. There is a significantly greater risk for arthritis to subsequently develop in the adjoining vertebrae.
- Artificial disk - an artificial disk is inserted; it replaces the cushion between two vertebrae.
- Discectomy (partially removing a disk) - a portion of a disk may be removed if it is irritating or pressing against a nerve.
- Partially removing a vertebra - a small section of a vertebra may be removed if it is pinching the spinal cord or nerves.
Complementary therapies
A large number of patients opt for complementary therapies, as well as conventional treatments; some opt just for complementary therapies.
According to the National Health Service (NHS), UK, chiropractic, osteopathy, shiatsu and acupuncture may help relieve back pain, as well as encouraging the patient to feel relaxed.
- An osteopath specializes in treating the skeleton and muscles.
- A chiropractor treats joint, muscle and bone problems - the main focus being the spine.
- Shiatsu, also known as finger pressure therapy, is a type of massage where pressure is applied along energy lines in the body. The shiatsu therapist applies pressure with his/her fingers, thumbs and elbows.
- Acupuncture, which originates from China, consists of inserting fine needles and specific points in the body. Acupuncture can help the body release its natural painkillers - endorphins - as well as stimulating nerve and muscle tissue.
TENS (transcutaneous electrical nerve stimulation) - a popular therapy for patients with chronic (long-term) back pain. The TENS machine delivers small electric pulses into the body through electrodes that are place on the skin. Experts believe TENS encourages the body to produce endorphins, and may possibly block pain signals returning to the brain. Studies on TENS have provided mixed results; some revealed no benefits, while others indicated that it could be helpful for some patients.
A TENS machine should be used under the direction of a doctor or health care professional.
Pregnant women, people with epilepsy, people with a pacemaker, and patients with a history of heart disease should not use a TENS machine.
Prevention of back pain
Steps to lower the risk of developing back pain consist mainly of addressing some of the risk factors.Exercise - regular exercise helps build strength as well as keeping your body weight down. Experts say that low-impact aerobic activities are best; activities that do not strain or jerk the back. Before starting any exercise program, talk to a health care professional.
- Core-strengthening exercises; exercises that work the abdominal and back muscles, help strengthen muscles which protect your back.
- Flexibility - exercises aimed at improving flexibility in your hips and upper legs may help too.
Body weight - the fatter you are the greater your risk of developing back pain. The difference in back pain risk between obese and normal-weight individuals is considerable.
Posture when standing - make sure you have a neutral pelvic position. Stand upright, head facing forward, back straight, and balance your weight evenly on both feet - keep your legs straight.
Posture when sitting - a good seat should have good back support, arm rests and a swivel base (for working). When sitting try to keep your knees and hips level and keep your feet flat on the floor - if you can't, use a footstool. You should ideally be able to sit upright with support in the small of your back. If you are using a keyboard, make sure your elbows are at right-angles and that your forearms are horizontal.
Lifting things - the secret for protecting your back when lifting things is to think "legs not back". In other words, use your legs to do the lifting, more than your back. Keep your back as straight as you can, keep your feet apart with one leg slightly forward so you can maintain balance, bend only at the knees, hold the weight close to your body, and straighten the legs while changing the position of your back as little as possible. Bending your back initially is unavoidable, when you bend your back try not to stoop or squat, tighten your stomach muscles so that your pelvis is pulled in. Most important, do not straighten your legs before lifting; otherwise you will be using your back for most of the work.
Do not lift and twist at the same time. If something is particularly heavy, see if you can lift it with someone else. While you are lifting keep looking straight ahead, not up nor down, so that the back of your neck is like a continuous straight line from your spine.
Moving things - remember that it is better for your back to push things across the floor, rather than pulling them.
Shoes - flat shoes place less of a strain on the back.
Driving - it is important to have proper support for your back. Make sure the wing mirrors are properly positioned so you do not need to twist. The pedals should be squarely in front of your feet. If you are on a long journey, have plenty of breaks - get out of the car and walk around.
Your bed - you should have a mattress that keeps you spine straight, while at the same time supporting the weight of your shoulders and buttocks. Use a pillow, but not one that forces your neck into a steep angle.
No comments:
Post a Comment